What is ADHD and how does it differ from ADD?
Today, we delve into the complex world of Attention Deficit Hyperactivity Disorder, or ADHD, and its relationship with Attention Deficit Disorder (ADD). There are a few misconceptions around this condition, so this article will explore what ADHD is, how it is diagnosed and clarify some misconceptions that are frequently seen.
As an example, ADD is no longer a standalone diagnosis but is now considered a part of ADHD, with varying levels of hyperactivity.
The Science Behind ADHD
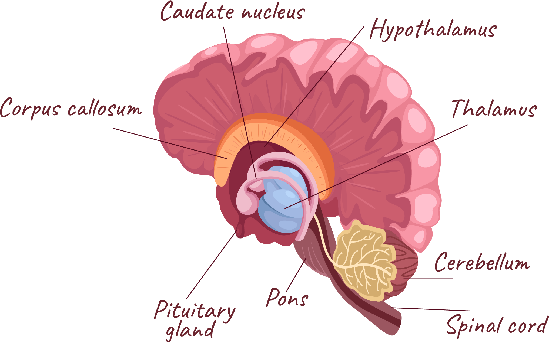
Neurobiology: ADHD and ADD are primarily disorders of the brain. Research has shown that individuals with these conditions have differences in brain structure and function that often involve those areas responsible for attention, impulse control, and executive functioning. Neuroimaging studies have revealed an overall reduction in brain size partially in the areas that control these functions namely the prefrontal cortex, caudate nucleus, corpus callosum and cerebellar vermis (Rege, 2023).
Genetics:
These conditions have a strong genetic link. If a parent or sibling has ADHD, the risk of a child developing it is significantly higher, with heritability estimates in the range of 60%–90% (Thapar et al., 2018). However, environmental factors can also contribute to the development of these disorders.
Neurotransmitters:
ADHD often involves imbalances in neurotransmitters like dopamine and norepinephrine, which regulate attention and impulse control (Rege, 2023). Medications prescribed for ADHD aim to correct these imbalances and improve symptoms.
Misconception: Its Just Laziness
ADHD has nothing do with laziness. It’s a neurobiological condition affecting attention and organisation.
How is ADHD or ADD diagnosed?
Diagnosing ADHD and ADD is a complex process requiring a comprehensive evaluation by a healthcare professional based on specific diagnostic criteria as described in the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders)
In children, a psychiatric interview is conducted with the parents and the child, for example the Diagnostic Interview for ADHD in young people – Young DIVA - is used in combination with Rating scales including the Conners’ Rating Scale, and Strengths and Difficulties Questionnaires. In contrast,in adults, the ASRS (Adult ADHD Self-Report Scale), and a psychiatric interview, for example the DIVA (Diagnostic Interview for ADHD In Adults), are used. Typically, it is a combination of the relevant diagnostic scales and a structured psychiatric interview that leads to a diagnosis (AADPA, 2022).
It is important to note that while an adult can be diagnosed with ADHD, symptoms must be present in childhood to receive the diagnosis. Psychologists and Psychiatrists look at past school reports and talk to parents to ascertain if the symptoms were present.
Misconception: ADHD and ADD are two distinct diagnoses
In fact, they are the same. The condition’s name changed in 1987 when hyperactivity was included. The diagnosis is now known as ADHD; however, an individual will fall into one of three types: predominately inattentive, predominately hyperactive/ impulsive, and combined (Anderson, 2023).
Some benefits of diagnosis
- An in-depth evaluation of someone’s memory, attention, and other aspects of their learning.
- Many mental health conditions have symptoms that mimic ADHD, and it is important to rule out other conditions.
- Many people with ADHD have another mental health condition that can impact their functioning in life.
- Understanding how ADHD symptoms impact cognitive, academic, social, and occupational functioning can help with planning interventions.
ADHD in Different Age Groups
ADHD is a kaleidoscope of behaviours stemming from a whirlwind of brain activities. The intensity of different behaviours varies significantly, painting a very unique picture for each individual. ADHD also differs from childhood to adulthood.
In children, ADHD may manifest as disruptive behaviour, an inability to stick to one task, and hyperactivity.
Adults with ADHD, on the other hand, often grapple with organisational challenges
and task execution, with or without the accompanying hyperactivity. However, it is important to note that living with ADHD is not all negative; with the right guidance, this energy can be channelled into creativity and productivity.
Gender and ADHD
Dealing with ADHD goes beyond age; it involves recognising the subtleties of gender. Historically, ADHD has been more frequently diagnosed in boys, who tend to exhibit symptoms leaning toward the more “classical” presentation of ADHD, such as hyperactivity and disruptive behaviour. On the other hand, girls with ADHD may present milder, less disruptive symptoms, such as inattention and daydreaming, which can sometimes lead to missed or delayed diagnoses (Tee-Melegrito & Gepp).
What Next?
Here are some quick actions that can help adults and children:
- Break larger tasks down into bite-size pieces: This helps to keep your focus
on the overall goal and gives a sense of achievement every time a task is ticked off. - Incorporate movement: Exercise is associated with a boost in the brain’s neurotransmitters, including the chemicals (dopamine, serotonin and norepinephrine) that many people with ADHD are thought to run short on.
- Meditate: Engage in mindfulness based breathing to calm the nervous system and improve concentration over time.
References
AADPA. (2022, October 1). ADHD screening and identification. Australian ADHD Clinical Practice Guideline - Australian ADHD Professionals Association (AADPA) https:// adhdguideline.aadpa.com.au/identification/ screening-and-identification/ (ASRS).
Anderson, D. (2023, March 3).
What is the difference between ADD and ADHD? Child Mind Institute
https://childmind.org/article /what-is-the-difference-between-add-and adhd/
Rege, S. (2023, March 4). Neurobiology of attention deficit hyperactivity disorder (ADHD) - A Primer. Psych Scene Hub. https://psychscenehub.com/psychinsights/ neurobiology-of-adhd/
Tee-Melegrito, R. A. (n.d.). ADHD gender differences: Signs, diagnosis, and more. Medical News Today. https:// www.medicalnewstoday.com/articles/is-adhd-more-common-in-males-or-females
Thapar, A., From the MRC Centre for Neuropsychiatric Genetics and Genomics and the Division of Psychological Medicine and Clinical Neurosciences, Address correspondence to Dr. Thapar Freedman, R. (2018, August 16). Discoveries on the genetics of ADHD in the 21st Century: New findings and their implications. American Journal of Psychiatry. https://ajp.psychiatryonline.org/doi/10.1176/
Share


